NeoVision offers Diabetic Retinopathy Treatment

Incidence of Diabetic Retinopathy
14 million diabetics risk loss of sight without early treatment. Bleeding in the retina is a frequent cause of blindness in diabetic patients aged 20-64 years.
Definition of Diabetic Retinopathy
If you have diabetes mellitus, your body does not use and store sugar properly. High blood-sugar levels can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal blood vessels is referred to as diabetic retinopathy. The disorder usually occurs in both eyes. These changes may include microaneurysms, retinal hemorrhage, macular edema, development of new and leaky blood vessels, and vitreous hemorrhages etc. Diabetic retinopathy can seriously affect vision and, if left untreated, cause blindness.
Symptoms of Diabetic Retinopathy
Often there are no symptoms in the early stages of the disease. Vision may not change until the disease becomes severe. There is no pain either. Blurred vision may occur when the macula swells from the leaking fluid. If new vessels have grown on the surface of the retina, they can bleed into the eye, blocking vision. However, even in more advanced cases, the disease may progress a long way without symptoms.
Types of Diabetic Retinopathy
In a very broad sense, there are two types of diabetic retinopathy:
- Non-proliferative diabetic retinopathy (NPDR)
- Proliferative diabetic retinopathy (PDR)
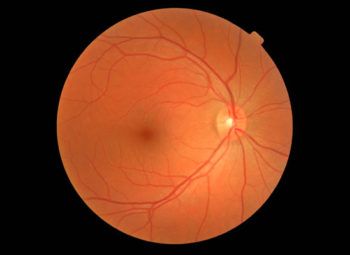
Early Diabetic Retinopathy with Microhemorrhages
NPDR, commonly known as background retinopathy, is an early stage of diabetic retinopathy. In this stage, tiny blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to swell or to form deposits called exudates. The beginning stages of diabetic retinopathy may cause blurriness in your central or peripheral (side) vision, or it may produce no visual symptoms at all. It mainly depends on where the blood vessel changes are taking place in your retina. Many people with diabetes have mild NPDR, which usually does not affect their vision. When vision is affected it is the result of macular edema and/or macular ischemia. Macular edema is swelling, or thickening, of the macula, a small area in the center of the retina that allows you to see fine details clearly. The swelling is caused by fluid leaking from retinal blood vessels. It is the most common cause of visual loss in diabetes. Vision loss may be mild to severe, but even in the worst cases, peripheral vision continues to function. Macular ischemia occurs when small blood vessels (capillaries) close. Vision blurs because the macula no longer receives sufficient blood supply to work properly.
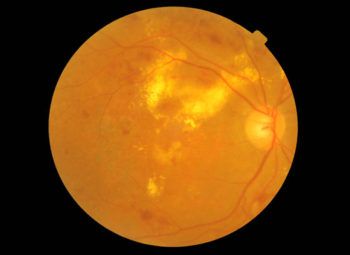
PDR is present when abnormal new vessels (neovascularization) begin growing on the surface of the retina or optic nerve. The main cause of PDR is the widespread closure of retinal blood vessels, preventing adequate blood flow. The retina responds by growing new blood vessels in an attempt to supply blood to the area where the original vessels closed. Unfortunately, the new, abnormal blood vessels do not re-supply the retina with normal blood flow. The new vessels are often accompanied by hemorrhage, scar tissue that may cause wrinkling or detachment of the retina. PDR may cause more severe vision loss than NDPR because it can affect both central and peripheral vision.
If you have diabetes this does not necessarily mean that your sight will be affected, but there is a higher risk. If your diabetes is well controlled then you are less likely to have problems, or they may be less serious. Evidence also suggests that such factors as pregnancy, high blood pressure and smoking may cause diabetic eye disease to develop or worsen. As a diabetic, or a person at risk, it is important that you take steps to help prevent the development of diabetic retinopathy by taking your prescribed medication as instructed; following a proper diet; exercising regularly; and having your eyes examined regularly. By doing so, chances are good that you can enjoy a lifetime of good vision and health.
Remember that if your vision is getting worse, this does not necessarily mean you have diabetic retinopathy. It may simply be a problem that can be corrected by glasses.
Detection of Diabetic Retinopathy
Since this disease can cause blindness, early diagnosis and treatment are essential. If you have diabetes or you have a family history of diabetes, you should have your eyes examined at least once a year by an ophthalmologist. During a thorough, comprehensive eye examination, your doctor gets to know you, your family history, your lifestyle and your vision needs. Your eyes will be dilated during the exam. To detect diabetic retinopathy, your ophthalmologist looks inside your eyes with an instrument called an ophthalmoscope. The interior of your eyes may also be photographed to monitor the progression of the disease.
Treatment of Diabetic Retinopathy
The best treatment is to prevent the development of retinopathy as much as possible. Strict control of your blood sugar will significantly reduce the long-term risk of vision loss from diabetic retinopathy. If high blood pressure and kidney problems are present, they need to be treated as well.
Your ophthalmologist may suggest laser surgery in which a strong light beam is aimed onto the retina to shrink the abnormal vessels. Laser surgery has been proved to reduce the risk of severe vision loss from this type of diabetic retinopathy by 60 percent. If you have macular edema, laser surgery may also be used. In this case, the laser beam is used to seal the leaking blood vessels. Multiple laser treatments over time are sometimes necessary. However, laser surgery often cannot restore vision that has already been lost. That is why finding diabetic retinopathy early is the best way to prevent vision loss.
Prevention of Diabetic Retinopathy
If you have diabetes, it is important to know that today, with improved methods of diagnosis and treatment, only a small percentage of people who develop retinopathy have serious vision problems. Early detection of diabetic retinopathy is the best protection against loss of vision. You can significantly lower your risk of vision loss by maintaining strict control of your blood sugar and visiting your ophthalmologist regularly.
If you are concerned about diabetic retinopathy and would like to schedule an eye appointment with NeoVision Eye Center, please contact us at 510-431-5511 (Union City).