NeoVision offers Glaucoma Treatment
Definition of Glaucoma
Glaucoma is a group of eye diseases that damage the optic nerve which connects the eye to the brain. The optic nerve is the main carrier of visual information to the brain. The optic nerve is made up of a huge number of nerve fibers, like an electric cable containing a huge number of wires. Glaucoma can damage these nerve fibers, causing blind spots to develop. When sufficient fibers have been lost or damaged, vision may be affected, first by loss of side vision and then later the loss of fine vision in the center. Usually, people don’t notice these blind areas until much optic nerve damage has already occurred. Blindness results if the entire nerve is destroyed.
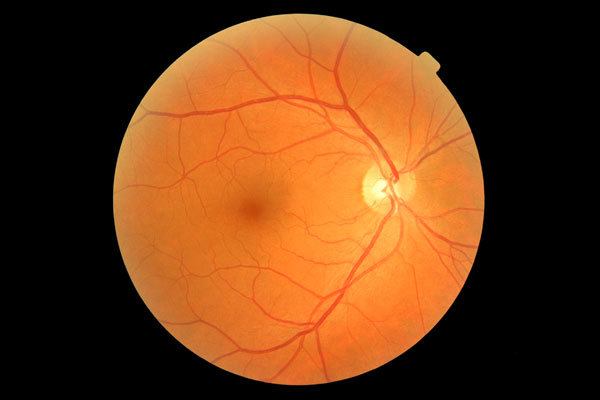
Normal Eye
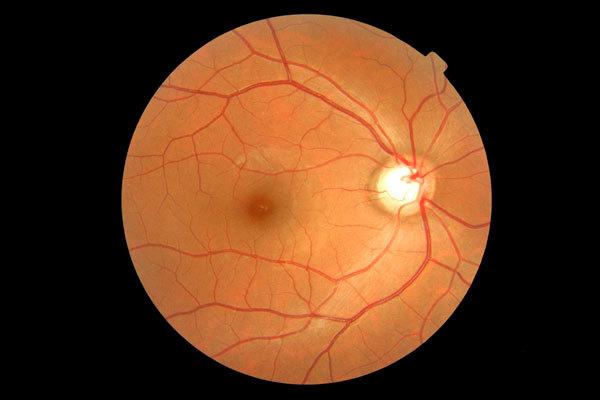
Glaucoma Suspect
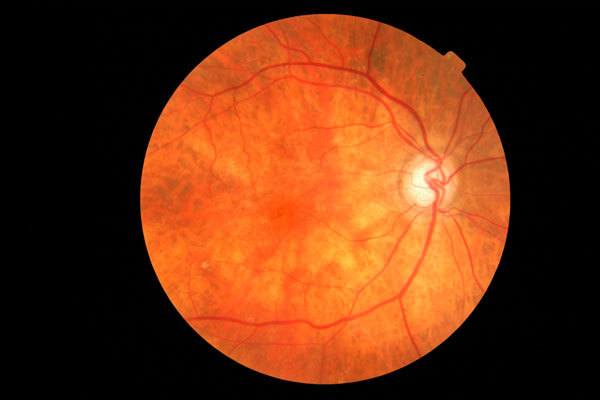
Advanced Glaucoma
Cause of Glaucoma
Clear fluid, called the aqueous humor, circulates inside the front portion of the eye. A small amount of this fluid is produced constantly, and an equal amount flows out of the eye through a microscopic drainage system, maintaining a constant level of pressure within the eye. Because the eye is a closed structure, if the drainage area for the aqueous humor (the drainage angle) is blocked, the excess fluid cannot flow out of the eye. Fluid pressure within the eye will increase, pushing against the optic nerve and potentially causing damage.
In some people, the damage to the optic nerve is caused by raised pressure. Others may have an eye pressure within normal limits but damage occurs because there is a weakness in the optic nerve. Glaucoma results when the pressure inside the eye is more than what the optic nerve can withstand. This pressure, if left untreated, can permanently damage the optic nerve causing progressively serious vision impairment.
The exact cause of glaucoma is not known, but if detected at an early stage and treated promptly, glaucoma can usually be controlled with little or no further vision loss. Regular eye exams offer the best chance for early diagnosis, as there are no symptoms of glaucoma until the disease is well advanced and irreversible damage has occurred.
Different Types of Glaucoma
There are four main types:
1. Chronic Open-angle Glaucoma
This is the most common form of glaucoma in the United States. The drainage angle of the eye becomes less efficient over time, and pressure within the eye gradually increases, which can damage the optic nerve. In some patients, the optic nerve becomes sensitive to normal eye pressure and is at risk for damage. Treatment is necessary to prevent further vision loss. Chronic open-angle glaucoma damages vision so gradually and painlessly that you are not aware of trouble until the optic nerve is already injured.
2. Angle-closure Glaucoma
Sometimes the drainage angle of the eye may become completely blocked. In the eye, the iris may drop over and completely close off the drainage angle. You can imagine this occurring much like a sheet of paper floating over a drain. If the paper suddenly drops over the opening, the flow is abruptly blocked. When eye pressure builds up suddenly, an acute angle-closure glaucoma attack occurs. Symptoms may include:
- Blurred vision
- Severe eye pain
- Headache
- Rainbow-colored halos around lights
- Nausea and vomiting
This is a true emergency. If you have any of these symptoms, call your ophthalmologist immediately. Unless this type of glaucoma is treated quickly, blindness can result. In some patients, glaucoma has features of both the chronic open-angle type and the acute angle-closure type. This may be called chronic angle-closure glaucoma or mixed mechanism glaucoma.
3. Secondary Glaucoma
They develop as a complication of other medical conditions. They are sometimes associated with eye surgery or advanced cataracts, eye injuries, certain eye tumors, or uveitis (eye inflammation). One type, known as pigmentary glaucoma, occurs when pigment from the iris flakes off and blocks the meshwork, slowing fluid drainage. A severe form, called neovascular glaucoma, is linked to diabetes. Also, corticosteroid drugs used to treat eye inflammations and other diseases can trigger glaucoma in a few people. Treatment is with medicines, laser surgery, or conventional surgery.
4. Developmental / Congenital Glaucoma
Some children are born with defects in the angle of the eye that slow the normal drainage of fluid. Children with this problem usually have obvious symptoms such as big, cloudy eyes, sensitivity to light, and excessive tearing. Surgery is usually the suggested treatment, because medicines may have unknown effects in infants and be difficult to give to them. The surgery is safe and effective. If surgery is done promptly, these children usually have an excellent chance of having good vision.
Incidence of Glaucoma
Some form of glaucoma affects about 2 in 100 people over the age of 40. Open-angle glaucoma, the most common form of glaucoma, affects about 3 million Americans, half of whom don’t know they have it. Glaucoma is the second most common cause of legal blindness in the United States and the leading cause of legal blindness in African-Americans.
It has no symptoms at first. But over the years it can steal your sight. With early treatment, you can often protect your eyes against serious vision problems.
Risk Factors for Glaucoma
Many individuals are at a higher risk to develop glaucoma. Following are the factors which increase the risk:
- Age: Chronic glaucoma becomes much more common with increasing age. It is uncommon below the age of 40 but affects one percent of people over this age and five percent over 65.
- Race: African Americans are at a higher risk of developing chronic glaucoma than other racial groups.
- Family: If you have a close relative who has chronic glaucoma then you should have regular eye examinations. You should advise other members of your family to do the same. This is especially true if you are over 40.
- Near-sightedness: People with a high degree of near-sightedness are more prone to chronic glaucoma.
- Systemic Diseases: It is believed that individuals with systemic diseases such as diabetes, anemia, or hardening of the arteries are at higher risk of developing glaucoma.
Detection of Glaucoma
Regular eye exams by your ophthalmologist are the best way to detect glaucoma. A glaucoma screening that checks only the pressure of the eye is not sufficient to determine if you have glaucoma. The only sure way to detect glaucoma is to have a complete eye exam. Your ophthalmologist will perform the following tests:
-
- Visual acuity: This eye chart test measures how well you see at various distances.
-
- Tonometry: This standard test determines the fluid pressure inside the eye using a tonometer. A tonopen is a portable, hand-held instrument that provides a safe, fast and accurate method of testing intraocular pressure.
- Gonioscopy: Inspection of drainage angle of your eye.
- Ophthalmoscopy: This examination provides your eye doctor with a better view of the optic nerve to check for signs of damage. To do this, your eye care professional places drops into the eye to dilate (widen) the pupil. An ophthalmoscope is an instrument that enables a doctor to examine the inside of your eye. After the examination, your close-up vision may remain blurred for several hours.
- Visual Field (Perimetry): This test measures your side (peripheral) vision. It helps your eye doctor to find out if you have lost side vision, a sign of glaucoma.
- HRT: This test analyzes the three-dimensional structure of your optic nerve.
- Pachymetry: This test measures the thickness of your cornea to evaluate the risk for glaucoma.
Treatment of Glaucoma
Treatment for glaucoma consists of eye medication to lower the pressure in the eye, laser treatment designed to make the “drain” of the eye function more efficiently, or surgery to create a new “drain” in order to lower pressure. Many patients will not have further loss of vision if the pressure is lowered sufficiently.
Glaucoma can usually be treated effectively by using eye drops or other medicines. In some cases, surgery may be necessary. Unfortunately, any loss of vision from glaucoma cannot usually be restored. But, early detection, prompt treatment, and regular monitoring can enable you to continue living in much the same way as you have always lived. Protect your eye health and your vision. Be sure to visit our office regularly.
Medicines
Medicines are the most common early treatment for glaucoma. They come in the form of eye drops and pills. Some cause the eye to make less fluid. Others lower pressure by helping fluid drain from the eye. Glaucoma drugs may be taken several times a day. Most people have no problems. However, some medicines can cause headaches or have side effects which affect other parts of the body. Drops may cause stinging, burning, and redness in the eye. Ask your eye doctor to show you how to put the drops into your eye. In addition, tell your ophthalmologist about other medications you may be taking before you begin glaucoma treatment.
Many drugs are available to treat glaucoma. If you have problems with one medication, tell your ophthalmologist. Treatment using a different dosage or a new drug may be possible. You will need to use the drops and/or pills as long as they help to control your eye pressure. This is very important. Because glaucoma often has no symptoms, people may be tempted to stop or may forget to take their medicine.
Laser Surgery
Laser surgery helps fluid drain out of the eye. In open-angle glaucoma, the drain itself is treated. The laser is used to modify the drain (trabeculoplasty). In angle-closure glaucoma, the laser creates a hole in the iris (iridotomy) to improve the flow of aqueous fluid to the drain. Although your ophthalmologist may suggest laser surgery at any time, it is often done after trying treatment with medicines. In many cases, you will need to keep taking glaucoma drugs even after laser surgery.
Laser surgery is performed in an ophthalmologist’s office or eye clinic. Before the surgery, your ophthalmologist will apply drops to numb the eye. As you sit facing the laser machine, your eye doctor will hold a special lens to your eye. A high-energy beam of light is aimed at the lens and onto the meshwork inside your eye. You may see flashes of bright green or red light. The laser makes 50-100 evenly spaced burns. These burns stretch the drainage holes in the meshwork. This helps to open the holes and lets fluid drain better through them.
Your ophthalmologist will check your eye pressure shortly afterward. You will be given some drops to take home for any soreness or swelling inside the eye. You will need to make several follow up visits to have your pressure monitored. Once you have had laser surgery over the entire meshwork, further laser treatment may not help. Studies show that laser surgery is very good at getting the pressure down. But its effects sometimes wear off over time. Two years after laser surgery, the pressure increases again in more than half of all patients.
SLT/YAG Tango Laser System
Here at Neovision, we use the best laser cataract technology available on the market. The Ellex Tango is without question the gold standard for SLT/Yag combo lasers around the world. This is the most desirable and most reliable SLT/Yag combination system on the market today.
Conventional Surgery
The purpose of surgery is to make a new opening for the fluid to leave the eye (trabeculectomy). Although your ophthalmologist may suggest it at any time, this surgery is often done after medicine and laser surgery has failed to control your pressure.
Surgery is performed in a clinic or hospital. Before the surgery, your eye surgeon gives you medicine to help you relax and then small injections around the eye to make it numb.
The surgeon then removes a small piece of tissue from the white (sclera) of the eye. This creates a new channel for fluid to drain from the eye. But surgery does not leave an open hole in the eye. The white of the eye is covered by a thin, clear tissue called the conjunctiva. The fluid flows through the new opening, under the conjunctiva, and drains from the eye.
You must put drops in the eye for several weeks after the operation to fight infection and swelling. The drops will be different than the eye drops you were using before surgery. You will also need to make frequent visits to your eye doctor. This is very important, especially in the first few weeks after surgery.
In some patients, surgery is about 80 to 90 percent effective at lowering pressure. However, if the new drainage opening closes, a second operation may be needed. Conventional surgery works best if you have not had previous eye surgery, such as a cataract operation.
Keep in mind that while glaucoma surgery may save remaining vision, it does not improve sight. In fact, your vision may not be as good as it was before surgery.
Like any operation, glaucoma surgery can cause side effects. These include cataract, problems with the cornea, inflammation or infection inside the eye, and swelling of blood vessels behind the eye. However, if you do have any of these problems, effective treatments are available.
If you are concerned about glaucoma and would like to schedule an eye appointment with NeoVision Eye Center, please contact us at 510-431-5511.











